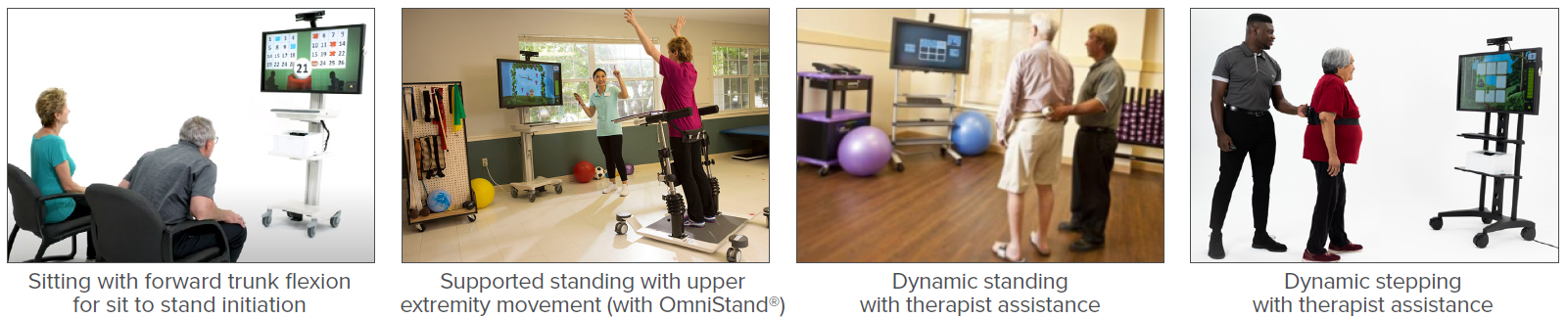
According to the CDC, more than one in four older adults fall each year. Falls may lead to fear of falling, decreased mobility, dependence, increased risk of future falls, and even death. The goal of a fall prevention and balance program is to decrease future falls and improve functional mobility, safety, and quality of life. Rehabilitation for those at risk of falling may include training for static and dynamic balance, gait, dual-task (DT) activity, and cognition which may be accomplished with virtual reality.
ACP - Accelerated Care Plus
Recent Posts
Virtual Reality in Fall Prevention
Topics: Fall Prevention & Balance, Clinical Tip
Pain*
Is your resident experiencing pain?
• Always assess pain level
• If resident is in pain, report immediately
Topics: Fall Prevention & Balance
Decreasing Pain and Improving Strength Using Ultrasound, Electrical Stimulation, and Exercise

Patient Information: Female, Age 80
Diagnosis: Subluxed Humerus / Pain
History:
This woman, a long-term care resident of a skilled nursing facility, was referred for rehabilitation services to address pain, decreased strength, and impaired motion of the left shoulder after experiencing a fall which caused her left shoulder to become partially dislocated (subluxed). Prior to her fall, she was able to dress independently.
Topics: Pain Management, Patient Success Story
Improving Activity Tolerance and Functional Mobility Using Breathing Therapy and Exercise

Patient Information: Female, Age 64
Diagnosis: Acute Respiratory Failure / COVID-19 / Chronic Obstructive Pulmonary Disease (COPD)
Topics: Patient Success Story, Cardiopulmonary
Improving Walking and Self-Care Using Exercise and Breathing Therapy with Biofeedback
Topics: Patient Success Story
Improving Swallowing Ability Using sEMG, Electrical Stimulation, and Exercise
Patient Information: Male, Age 71
Diagnosis: Subdural Hematoma / Oropharyngeal Dysphagia
History:
This gentleman was admitted to a skilled nursing facility for rehabilitation services following hospitalization due to a fall, which resulted in a traumatic subdural hematoma (bleeding between the skull and brain). He was then diagnosed with encephalopathy (damage to the brain) and oropharyngeal dysphagia (difficulty swallowing), with a feeding tube placed during his hospitalization to provide nutrition and hydration. Prior to his accident, this gentleman consumed a regular diet and drank thin liquids.
Topics: Dysphagia, Patient Success Story
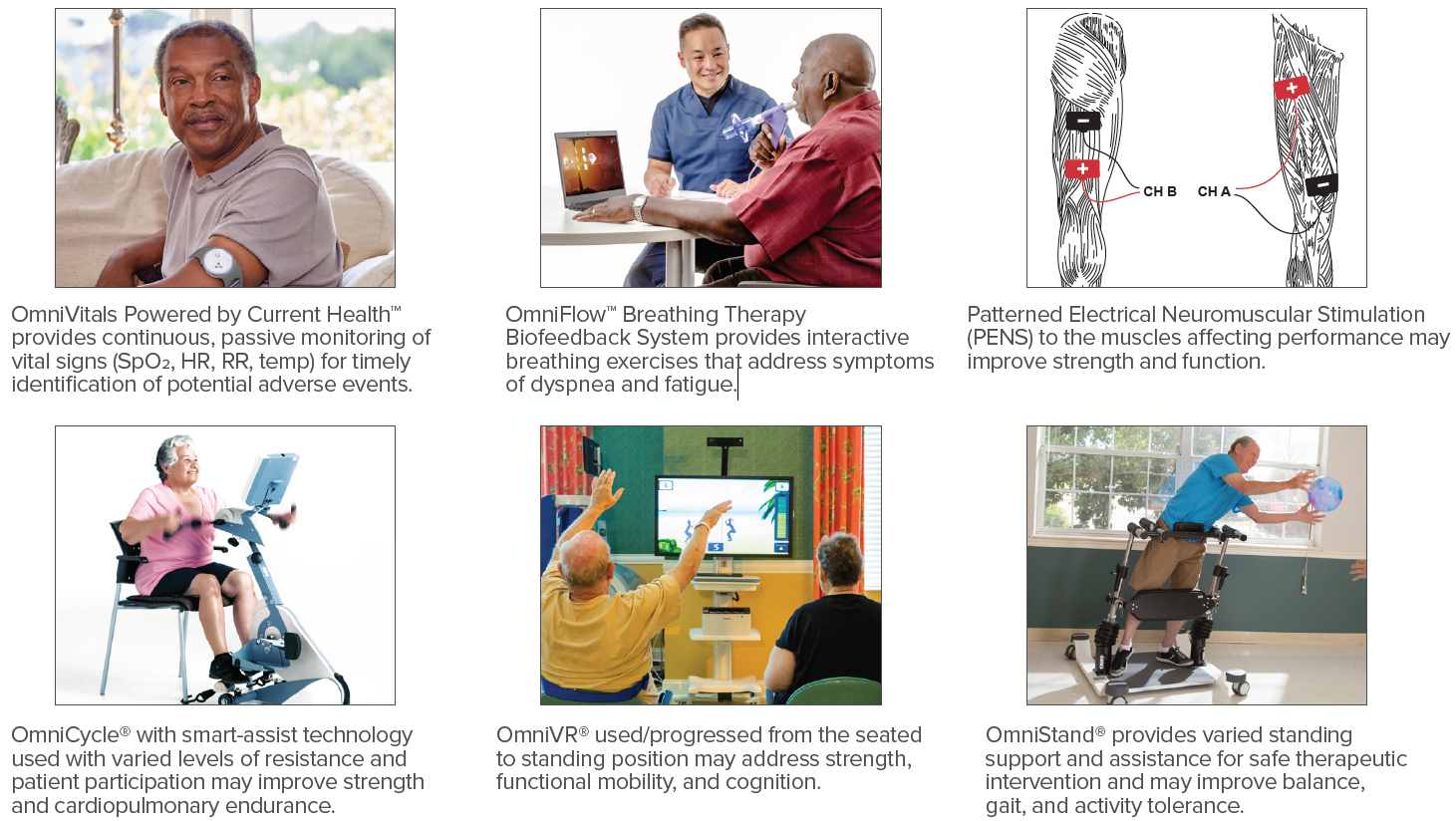
Rehabilitation in Individuals with Long COVID
According to the CDC, in the U.S. there have been more than 33.9 million cases since January 2020. As many as 1 in 10 of those who develop COVID-19 exhibit new and prolonged symptoms lasting 12 weeks or longer. This is known as long COVID and occurs regardless of the severity of the acute illness. These individuals may have multisystem involvement with the most common symptoms after 6 months being fatigue, post-exertional symptom exacerbation (PESE), and problems with memory and concentration (brain fog). Therapists should screen for PESE, a worsening of symptoms typically 12 to 48 hours following even minimal cognitive, physical, emotional, or social activity that may last for days or weeks. (World Physiotherapy, 2021)
Topics: Clinical Tip, Cardiopulmonary
Interdisciplinary Fall Prevention for Geriatrics
In a recent CDC Morbidity and Mortality Weekly Report, Moreland & Lee (2021) analyzed 2018 U.S. data which revealed individuals 65 and older had 2.4 million emergency department visits and more than 700,000 hospitalizations due to unintentional injuries. Greater than 90% of these injuries were related to falls. This shows the importance of an effective interdisciplinary fall prevention and balance program for the geriatric population.
Topics: Fall Prevention & Balance, Clinical Tip
Improving Speech and Swallowing Using sEMG and Breathing Therapy with Biofeedback
Patient Information: Female, Age 78
Diagnosis: Oral Cancer / Dysarthria / Oropharyngeal Dysphagia
History: This woman, a long-term care resident of a skilled nursing facility, has a history of oral cancer four years ago. At that time, she underwent removal of 50% of her tongue, tissue grafting for her palate, and has resultant decreased jaw movement, oropharyngeal dysphagia (difficulty swallowing), and dysarthria (difficulty with speech production). Additionally, she underwent a tracheostomy (tube inserted into the trachea to assist with breathing) and a feeding tube was placed to provide nutrition due to her inability to eat and drink by mouth. She has received intermittent speech-language pathology services over the four years. Prior to her cancer, this woman had no limitations in eating, drinking, and speaking.
Topics: Dysphagia, Patient Success Story, Speech Rehab
Improving Swallowing Ability using sEMG and Exercise
Patient Information: Female, Age 66
Diagnosis: Hemorrhagic Stroke / Oropharyngeal Dysphagia
History: This woman was admitted to a skilled nursing facility for rehabilitation services following hospitalization due to suffering a hemorrhagic stroke. As a result, she was diagnosed with altered mental status and oropharyngeal dysphagia (difficulty swallowing) and a feeding tube was placed to provide nutrition and hydration. Prior to her stroke, this woman ate a regular diet and drank thin liquids.
Topics: Dysphagia, Patient Success Story