This 65-year-old gentleman was admitted to Quince Nursing and Rehabilitation Center in Memphis, TN for rehabilitation services following hospitalization due to a stroke. He was diagnosed with oropharyngeal dysphagia (difficulty swallowing). His swallow initiation was inconsistent, and he had difficulty managing his own secretions. He could not take any food or liquid by mouth and a feeding tube was placed. Prior to his stroke, he ate a regular diet.
Read More
Topics:
Dysphagia,
Patient Success Story
Barikroo, A., Im, I., Crary, M., Carnaby, G. (2023). Effects of Age and Lingual-Palatal Pressure Levels on Submental Surface Electromyography Measures. Dysphagia. doi.org/10.1007/s00455-023-10553-6
Read More
Topics:
Dysphagia,
Speech Rehab,
SLP Clinical Connection
Galek, K.E., Bice, E.M., Allen, K. (2023). The Influence of Three Feedback Conditions on Performing a Swallow Motor Pattern in Healthy Adults. Folia Phoniatrica et Logopaedica (Karger). doi.org/10.1159/000525634
Read More
Topics:
Dysphagia,
Speech Rehab,
SLP Clinical Connection
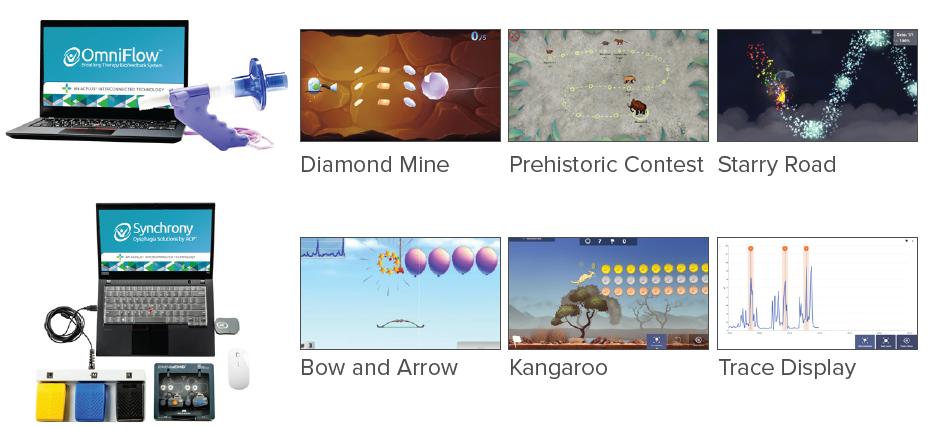
Improving Speech Using Breathing Therapy with Biofeedback
Speech Therapy: (3x/week x 11 weeks)
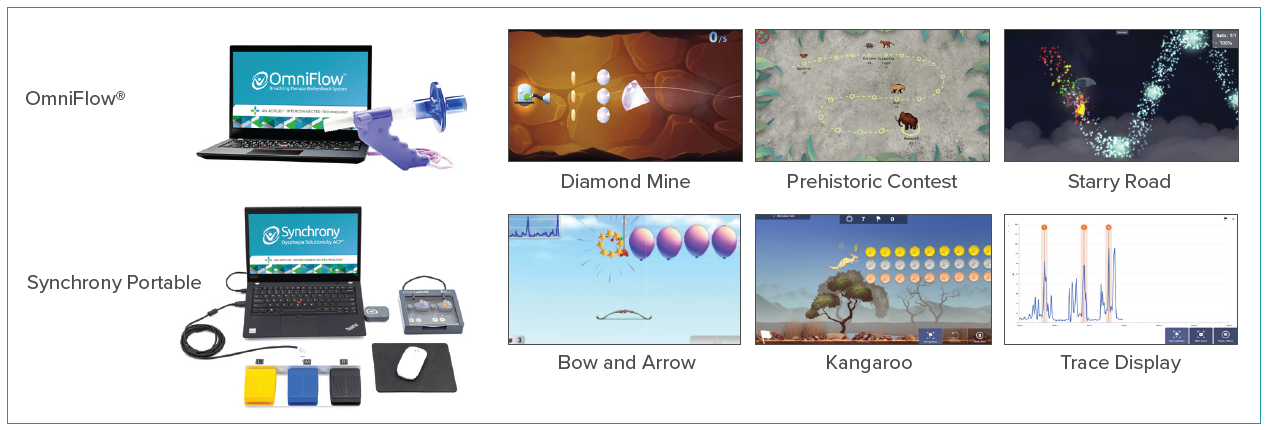
OmniFlow® Breathing Therapy Biofeedback
• Airway clearance – The Dandelion
• Forced expiration – Prehistoric Contest
• Respiratory muscle training – Starry Road
Read More
Topics:
Dysphagia,
Speech Rehab,
SLP Clinical Connection
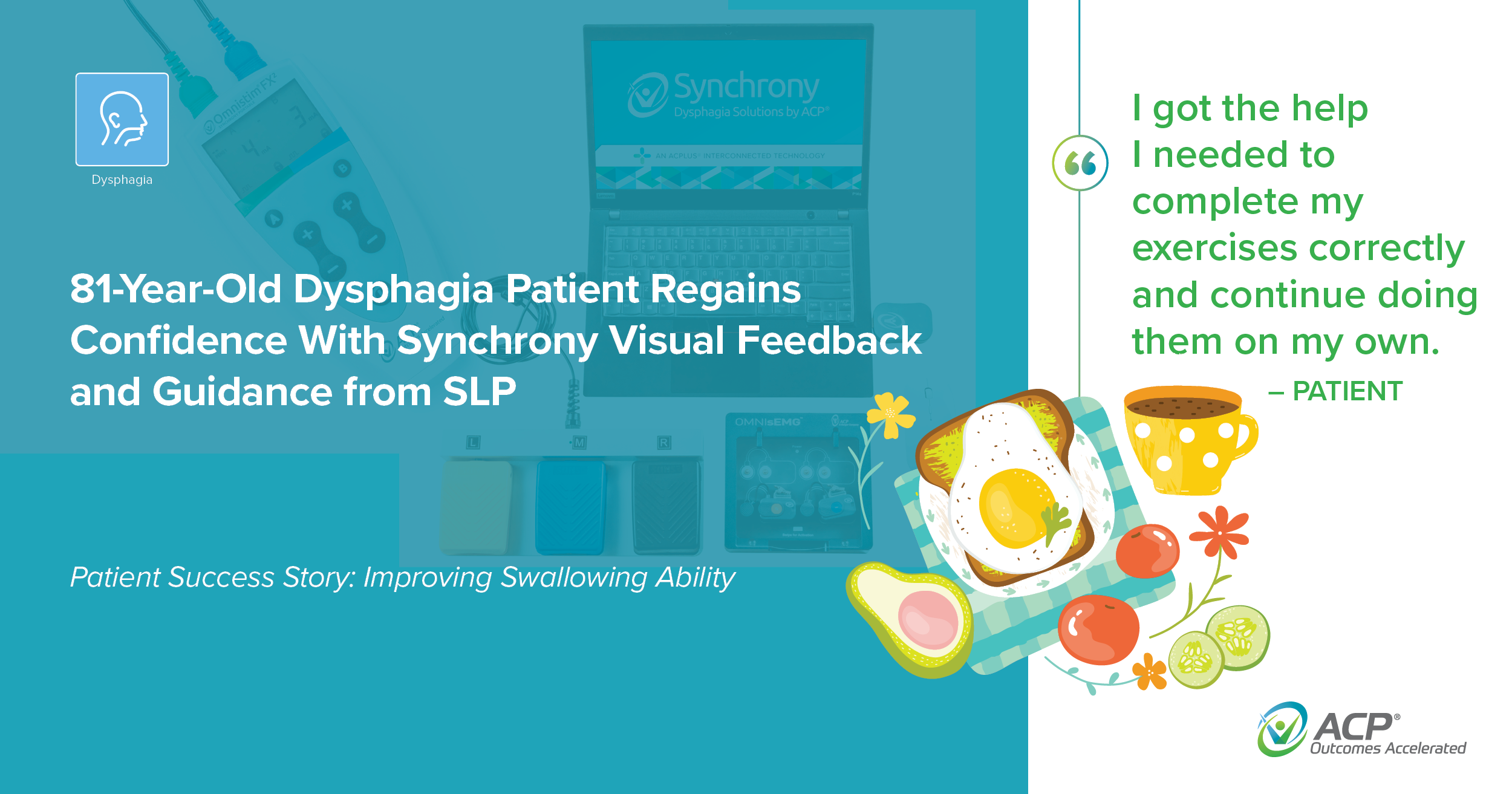
This 81-year-old woman was admitted to a skilled nursing facility following hospitalization for acute respiratory failure. She was intubated (tube inserted in airway to assist with breathing), had pneumonia caused by aspiration (material entering the lungs), and oropharyngeal dysphagia (difficulty chewing and swallowing). As a result, she was referred for speech language pathology (SLP) services. Although she had a history of dysphagia from previous spinal surgery, she was able to consume a diet of regular food and thin liquids prior to this hospitalization.
Read More
Topics:
Dysphagia,
Patient Success Story
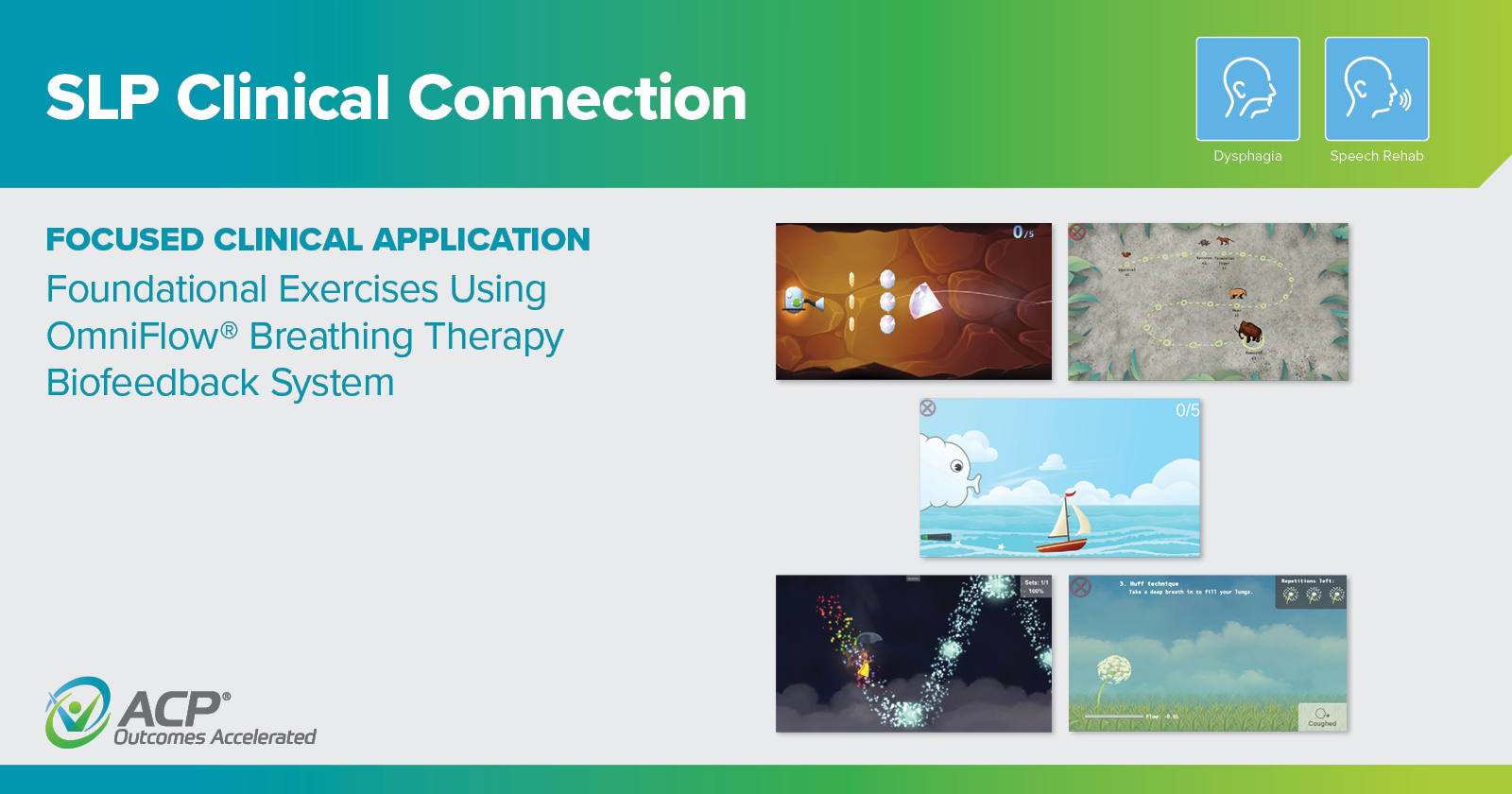
Foundational Exercises Using OmniFlow® Breathing Therapy Biofeedback System
Read More
Topics:
Dysphagia,
Speech Rehab,
SLP Clinical Connection