Speech-language pathologists (SLPs) are commonly involved in the rehabilitation of patients with cardiopulmonary disorders. Patients hospitalized with respiratory diseases such as COPD and heart failure (HF) are identified as at risk for development of oropharyngeal dysphagia. Additionally, patients who experience prolonged endotracheal intubation have an increased risk of developing dysphagia. (Malandraki et al., 2016) This is often seen in patients hospitalized for COVID-19.
Speech-Language Pathologist and the Use of Advanced Technology in Cardiopulmonary and Airway Disorders
Topics: Dysphagia, Cardiopulmonary
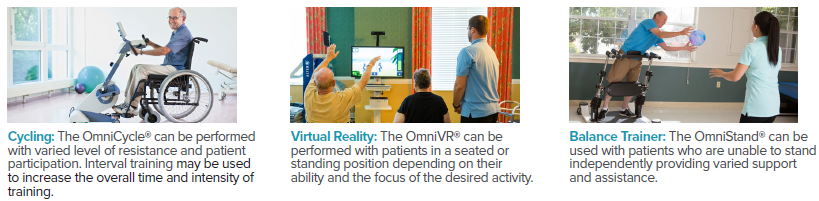
Cycling Exercise in Rehabilitation to Improve Coordination and Normalize Muscle Tone
Physical and occupational therapists treat many individuals who present with impaired coordination, motor control, balance and tone. These individuals may have a wide range of diagnoses, from neurologically involved, such as cerebral vascular accident (CVA) and Parkinson’s disease, to orthopedic involvement such as post-total knee replacement (TKR). The common goal of improving functional mobility and outcomes may be achieved by the addition of research-supported cycling and biophysical agents.
Topics: Clinical Tip, Cardiopulmonary, Neuro Rehab
Patient Information: Female, Age 72
Diagnosis: Cardiac Arrest / Pulmonary Embolism
History: This woman was referred to a skilled nursing facility for rehabilitation services due to severe weakness and debility following hospitalization. She had a pulmonary embolism (blood clot in the lungs) which required intubation and life support with extracorporeal membrane oxygen – ECMO (blood pumped outside the body to a heart and lung machine to remove carbon dioxide and send oxygenated blood back to the body). Prior to hospitalization, she lived at home and was independent with all mobility and self-care.
Topics: Patient Success Story, Cardiopulmonary
The rehabilitation of patients with and recovering from COVID-19 is evolving and will be an integral part of therapy for the foreseeable future. The American Physical Therapy Association (APTA) developed a task force representing all academies and sections to identify core outcome measures to be used with all patients diagnosed with COVID-19 throughout care, across all settings. These outcome measures are to be used with patients having goals associated with five constructs; function, strength, endurance, cognition, and quality of life. (APTA, 2020)
Topics: Clinical Tip, Cardiopulmonary
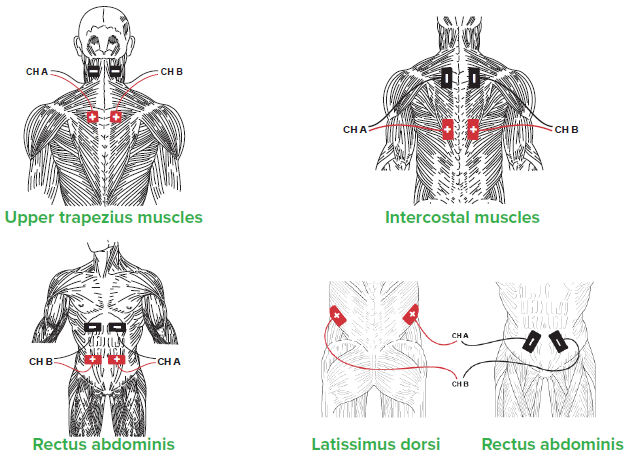
Improving Strength and Functional Mobility Using Electrical Stimulation and Exercise
Patient Information: Female, Age 68
Diagnosis: Respiratory Failure
History: This woman was referred to a skilled nursing facility due to severe deconditioning following a two-month hospitalization for pneumonia, during which she experienced respiratory arrest and required ventilation by tracheostomy intubation (surgical procedure inserting a breathing tube through the trachea to restore breathing).
Topics: Patient Success Story, Cardiopulmonary
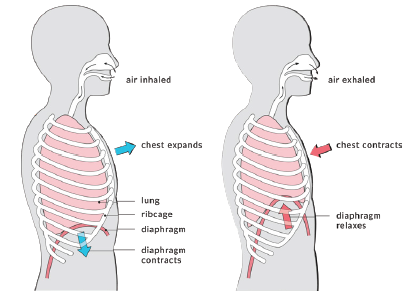
Diaphragmatic Breathing Exercise and Patterned Electrical Neuromuscular Stimulation (PENS)
Diaphragmatic breathing helps individuals use their diaphragm correctly while breathing and enhances oxygen exchange (Cleveland Clinic, 2020). With age, stress, poor posture, and illness breathing changes and becomes shallow with increased reliance on accessory muscles. Implementing diaphragmatic breathing may help improve oxygen delivery throughout the body, use less effort and energy to breathe, and decrease overall oxygen demand.
Topics: Clinical Tip, Cardiopulmonary
Achieving Independent Functional Mobility with Electrical Stimulation, Diathermy and Exercise
Patient Information: Male, Age 69
Diagnosis: Chronic Heart Failure / Muscle Weakness / Kidney Failure
History: This man was admitted to a skilled nursing facility after a seven day hospital stay due to a decline in his ability to care for himself and his wife. He was referred to occupational and physical therapy to improve his strength and function, with the goal to return home and resume his role as the primary caregiver for his wife.
Topics: Patient Success Story, Cardiopulmonary
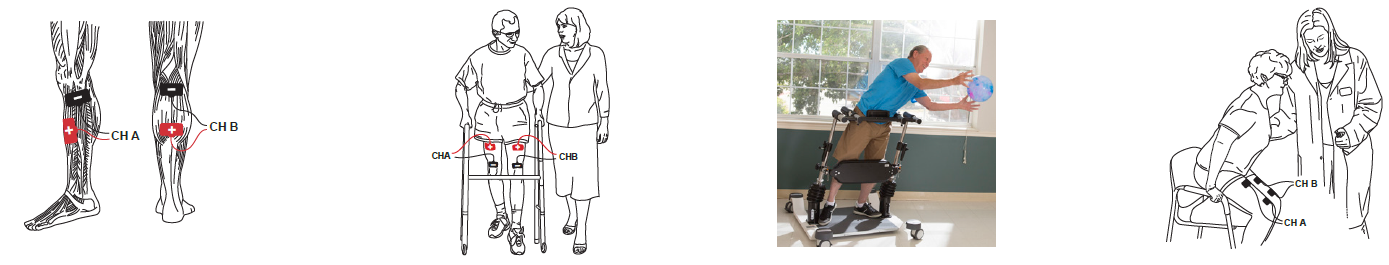
Improving Activation of Accessory Respiratory Muscles with NMES
Primary respiratory muscles during normal quiet breathing include the diaphragm and external intercostals. Accessory muscles of respiration assist the primary muscles when the chest is not expanding or contracting effectively to meet ventilation demands. Increased age, stress, poor posture, COPD, pneumonia, and illness are conditions that negatively impact proper oxygen and carbon dioxide exchange in the lungs.
Topics: Clinical Tip, Cardiopulmonary
Rehabilitation for Severe Deconditioning Using Advanced Technology and Electrical Stimulation
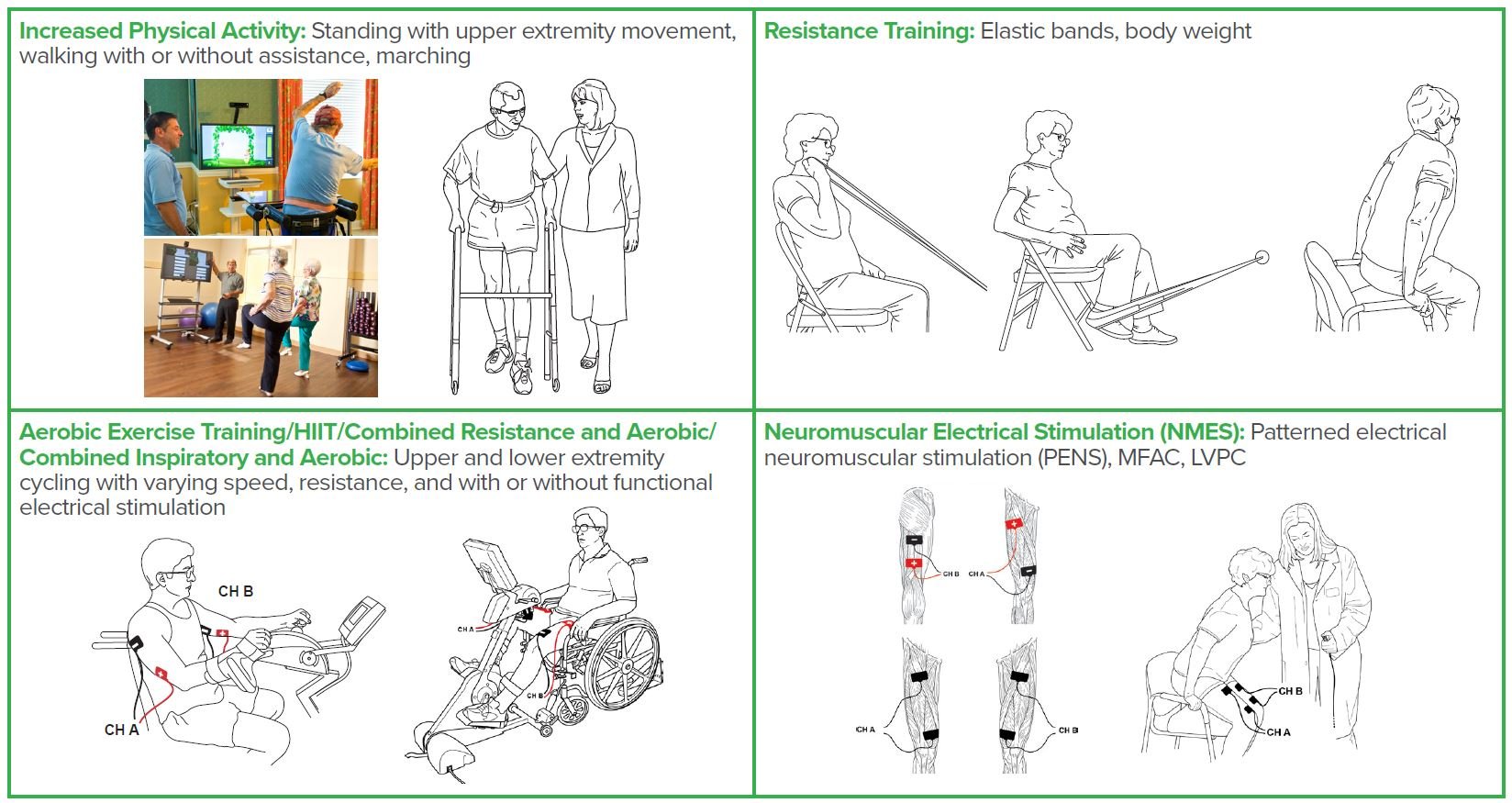
Individuals who present with a compromised pulmonary system, are acutely ill, or hospitalized for extended periods may become deconditioned or develop hospital-acquired muscle weakness, among other deleterious effects. Even healthy individuals may become deconditioned and frail if they decrease their activity level due to social distancing and limiting time outside their room or home.
Topics: Clinical Tip, Cardiopulmonary
Heart Failure Clinical Practice Guidelines Therapy Recommendations
Approximately 6.5 million adults in the United States have heart failure. Heart failure (previously referred to as chronic heart failure or CHF) occurs when the heart cannot pump enough blood throughout the body to meet the requirements of other organs and muscles. This results in a wide variety of symptoms and functional impairments which may result in hospitalization, re-hospitalization, and death. In 2017, heart failure contributed to 1 in 8 deaths. (CDC, 2020)
Topics: Clinical Tip, Cardiopulmonary