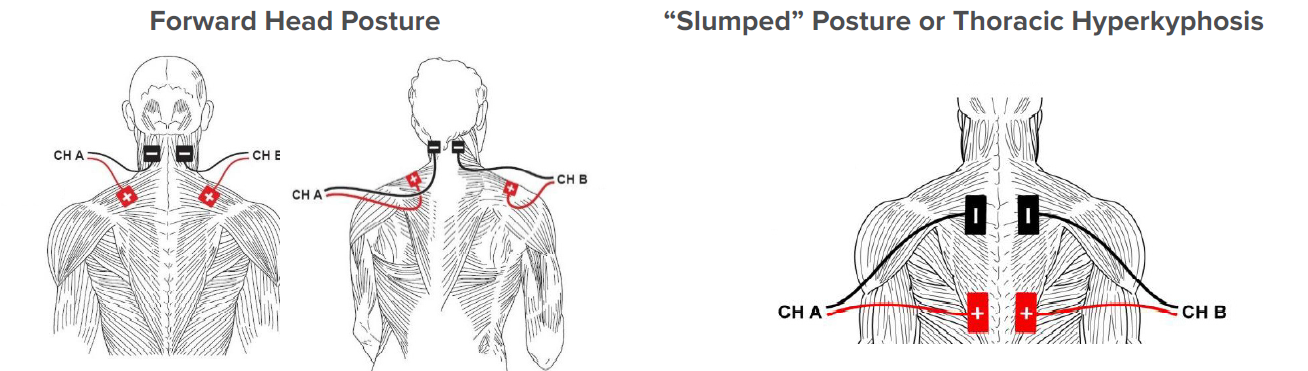
Shoulder range of motion, strength, and function are vital to self-care and everyday activities such as dressing, bathing, lifting and carrying items, and putting away groceries. With advanced age individuals may experience a variety of shoulder impairments including arthritis, rotator cuff tears, impingement, and fractures. These issues can result in pain, decreased motion, impaired strength, and reduced function.
ACP
Recent Posts
Shoulder Rehabilitation Using Isometrics and Biophysical Agents
Topics: Pain Management, Clinical Tip, Orthopedic
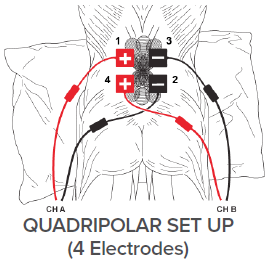
Traditional Interferential Current (IFC) or Premodulated (PREMOD) IFC for Pain Relief
IFC has been shown to be effective for treating multiple types of pain in locations throughout the body.1,2 Both traditional IFC and PREMOD IFC can be done at sensory and motor levels. Sensory settings provide segmental pain relief that is fast-acting and lasts for several hours. Motor stimulation tends to be slower-acting, but may relieve pain for up to 8 hours via segmental and systemic pain modulation. Available options in the OmniStim® Pro and OmniVersa® electrical stimulation devices include:
Topics: Pain Management, Clinical Tip
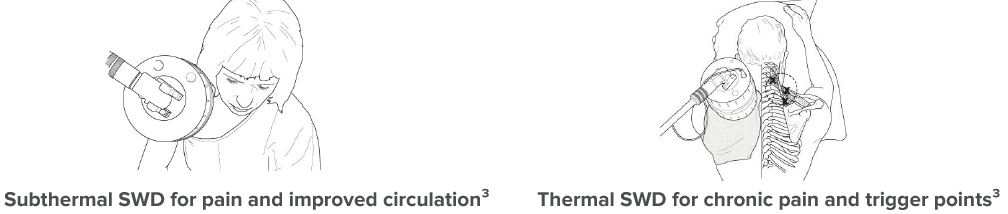
Decreasing Pain and Improving Function with Subthermal Diathermy and Exercise
Patient Information: Female, Age 82
Diagnosis: Right Hip Open Reduction Internal Fixation (ORIF) / Right Hip Pain / Falls
History: This woman was referred to a skilled nursing facility for rehabilitation services after hospitalization due to a fall which resulted in a hip fracture requiring surgery. Prior to her fall she lived independently at home.
Topics: Fall Prevention & Balance, Pain Management, Patient Success Story
Stroke is a common diagnosis in rehabilitation and resultant visual field disorders can be a significant barrier to a successful rehabilitation program.
Topics: Clinical Tip, Neuro Rehab
Improving Balance and Functional Mobility Using Dynamic Balance Training and Exercise
Patient Information: Male, Age 62
Diagnosis: Muscle Weakness / Falls / Dementia
History: This gentleman, a long-term skilled nursing facility resident, experienced several falls from his wheelchair and was referred to therapy by nursing to maximize his overall functional mobility in an effort to reduce his fall risk.
What do you do in your free time?
In my free time, I enjoy gardening, cooking, spending time with my three dogs and helping my stepdaughter with her extracurricular activities: raising a goat for FFA and racing her junior dragster.
How long have you been with ACP? I am celebrating one year with ACP this week!
What is your career background?
Before ACP, I was an art director working in ad agencies for high tech and healthcare clients. This is my first time to work in-house for a corporate marketing department.
Topics: Employee Spotlight
Improving Urinary Incontinence with Electrical Stimulation and Exercise
Patient Information: Female, Age 74
Diagnosis: Urinary Incontinence / Hip Fracture
History: This woman was admitted to a skilled nursing facility with significant decline in mobility
and function after an extended hospitalization due to a fall and subsequent fractured hip. Prior to her fall she lived at home with her family. Due to the severe decline in her function, she received rehabilitation services for one month prior to the continence program being added to her plan of care. Urinary incontinence had been an issue for years, but got significantly worse over the course of her hospitalization.
Optimizing Head, Neck and Trunk Positioning to Impact Swallow Performance and Safety
Topics: Dysphagia, Clinical Tip
Improving Urge and Stress Incontinence with Continence Improvement Pelvic Muscle Exercise
Patient Information: Female, Age 72
Diagnosis: Urge and Stress Incontinence
History: This woman, an independent living resident, referred herself to therapy for incontinence rehabilitation after attending a facility open house where she learned of the program. She reported gradual decreased control of urine with both stress incontinence (inability to hold back urine leakage with increases in abdominal pressure caused by laughing and sneezing) and urge incontinence (inability to stop unexpected and urgent urine flow) over the past year.
From 2012 through 2017, SNF occupancies fell from nearly 86% to less than 82%. This drop is associated with a number of factors, including the influence of Medicare Managed Care contracts navigating shorter length of stay in SNF, the impact of bundled payment models trying to constrain spend by reducing the time spent in inpatient PAC settings, and the growth in beneficiaries electing to bypass SNF to receive PAC services through home health. Overcoming these challenges to build census is comprised of two main components; attracting and providing superior quality outcomes to short-stay rehabilitation clients, and providing quality care and delivering an exceptional customer experience to maintain residential patients.
Topics: Industry News