As speech-language pathologists (SLPs) we often make diet recommendations. The unfortunate reality is we have scant information to direct these decisions. There is some evidence concerning the impact of volume and viscosity on swallowing kinematics (Barikroo, 2015; Chi-Fishman, 2002; Miller, 1996; Nagy, 2015; Watts, 2015). However, a systematic review (Steele, 2015) revealed little evidence to guide practice with respect to different degrees of modifying solid foods for patients with dysphagia. This means SLPs must rely on the sound understanding of the mastication process to make these decisions. Unfortunately, the system is quite complex and difficult to evaluate. This article represents the first of a series related to mastication that will address how mastication works and some possible assessment methods. Armed with this knowledge, SLPs may formulate more informed recommendations as part of a comprehensive patient care plan.
Ed M. Bice, M.Ed., CCC-SLP
Recent Posts
Your Wet Voice Makes Me Uncomfortable
In the previous two articles in this series we examined the evidence concerning the clinical indictors of coughing and a runny nose. The conclusion was, both indicators provide us with weak information concerning swallowing function. In this edition, the evidence for wet vocal quality as a meaningful clinical finding will be discussed.
Topics: Dysphagia
Hand Me a Tissue: Rhinitis in the Geriatric Population
Therapist have often relied upon “clinical signs” to assist in determining if a patient is experiencing aspiration. Those signs have included coughing (see "Cough Up The Facts"
previous blog post), throat clearing, wet vocal quality, runny nose, and many others. There is very little empirical evidence to support the correlation of “clinical signs” to an episode of aspiration. A runny nose is often considered to be a salient sign of aspiration; perhaps this is an over generalization.
Topics: Dysphagia
Speech Pathologists who treat dysphagia often rely on a patient’s cough as a marker of aspiration. Other healthcare professionals have been educated that coughing is a sign of swallowing difficulty. How accurate is this statement in the geriatric population and what are other reasons a patient may be exhibiting a cough?
Topics: Dysphagia
As speech language pathologists, we are all familiar with the word “competence.” After a good deal of time invested in educational pursuits followed by a nine-month period of supervision, we are awarded our Certificate of Clinical Competence (CCC) from the American Speech Language and Hearing Association (ASHA). The reality is, when I received my CCC, I could hardly consider myself competent in any area of practice.
Topics: Dysphagia
I am often surprised to learn that terms and concepts I use on a regular basis are different than
I thought. A common term that I have misunderstood for many years is “aspiration pneumonia.”
Recent reading has led me to a new understanding of this term.
Topics: Dysphagia
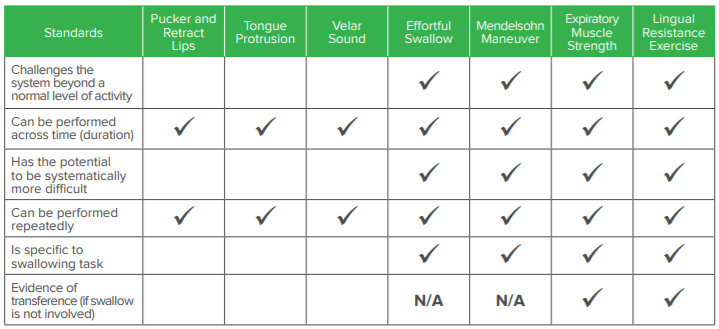
Exercise in Swallowing Therapy (Part 3 of a 3-Part Series)
This is the third and final installment of our “Exercise in Swallowing Therapy” series. This article will examine some commonly used interventions in light of exercise principles. But first, a quick review. In order to be considered an exercise the activity must meet certain criteria (for more information refer to the two previous articles).
Topics: Dysphagia
Exercise in Swallowing Therapy (Part 2 of a 3-Part Series)
In the first installment of “Exercise in Swallowing Therapy” the roles of overload and adequate
duration of therapy were discussed. In this second installment, additional exercise principles of intensity progression and repetition are described.
Topics: Dysphagia